Guideline
1 Page
Preview
Page 1
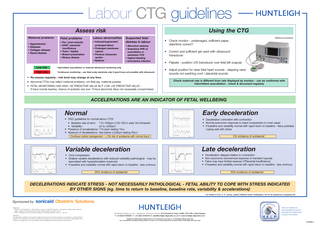
Labour CTG guidelines Using the CTG
Assess risk Maternal problems • Hypertension • Diabetes • Collagen disease • Renal disease
Fetal problems
Labour abnormalities
• Pre / post-maturity • IUGR / placental insufficiency • Twins / triplets • Breech presentation • Rhesus disease
• Induced/augmented/
Suspected fetal distress in labour
prolonged labour • Prolonged membrane rupture • Previous Caesarean section • Epidural
• Meconium staining • Suspicious FHR on auscultation or admission CTG • Vaginal bleeding • Intrauterine infection
Low risk
Intermittent auscultation or external ultrasound monitoring only
High risk
Continuous monitoring - use fetal scalp electrode only if good trace not possible with ultrasound
FM800Encore Fetal Monitor
• Check monitor : undamaged, sufficient paper, date/time correct? • Correct and sufficient gel used with ultrasound transducer • Palpate - position U/S transducer over fetal left scapula • Adjust position for clear fetal heart sounds - slapping valve sounds not swishing cord / placental sounds
• Re-assess regularly - risk level may change at any time. • Abnormal CTGs may reflect maternal problems, not fetal (eg. maternal pyrexia) • FETAL MONITORING HAS HIGH -VE PREDICTIVE VALUE BUT LOW +VE PREDICTIVE VALUE If trace normal reactive, chance of acidosis very low1. If trace abnormal, fetus not necessarily compromised.
Check maternal rate is different from rate displayed by monitor - can be confirmed with intermittent auscultation - check & document regularly
ACCELERATIONS ARE AN INDICATOR OF FETAL WELLBEING
Normal
Early deceleration
• FIGO guidelines for normal labour CTG2 • Baseline rate at term: 110-150bpm (120-160 in early 3rd trimester) • Variability : ±5 to ±25bpm • Presence of accelerations: ↑15+bpm lasting 15s+ • Absence of decelerations: See below (↓20bpm lasting 30s+)
• Deceleration coincident with contraction • Normal autonomic response to head compression in most cases • If baseline and variability normal with rapid return to baseline - fetus probably coping well with stress 5% incidence of acidaemia1
Continue routine management - < 2% risk of acidaemia with normal trace1
Variable deceleration
Late deceleration
• Cord compression • Shallow variable decelerations with reduced variability pathological - may be associated with hyperstimulation (oxytocin) • If baseline and variability normal with rapid return to baseline - less ominous
• • • •
Deceleration delayed relative to contraction Non-autonomic biochemical response to transient hypoxia Fetus may have limited reserves (?Placental insufficiency) If baseline and variability normal with rapid return to baseline - less ominous
25% incidence of acidaemia1
50% incidence of acidaemia1
DECELERATIONS INDICATE STRESS - NOT NECESSARILY PATHOLOGICAL - FETAL ABILITY TO COPE WITH STRESS INDICATED BY OTHER SIGNS (eg. time to return to baseline, baseline rate, variability & accelerations) Our thanks to Prof. D. K. James, Queen’s Medical Centre, Nottingham, UK for his assistance in preparing this
Sponsored by: sonicaid Obstetric Solutions References: 1 Steer P.J. and Daniellian P.J. ‘Fetal distress in Labor’ In: High Risk Pregnancy - Management Options (Eds: James D, Steer P, Weiner C and Gonik B) Publ: London, WB Saunders Ltd pp1077-1100 2 FIGO : Guidelines for the use of fetal monitoring. Int.J.Gynaecol.Obstet, 1987, 25 : 159-167. Disclaimer: The information contained in this poster is believed to be correct at the time of going to print based on current European guidelines. It is intended to be used as a guide only and does not cover all risk factors. It remains the responsibility of the clinician to manage each case in accordance with local guidelines and recommended clinical practice.
Huntleigh Healthcare Ltd. - Diagnostic Products Division 35 Portmanmoor Road, Cardiff, CF24 5HN, United Kingdom T: +44 (0)29 20485885 F: +44 (0)29 20492520 E: [email protected] W: www.huntleigh-diagnostics.com ®
Registered No: 942245 England. Registered Office: 310-312 Dallow Road, Luton, Beds, LU1 1TD ©Huntleigh Healthcare Limited 2009 and ™ are trademarks of Huntleigh Technology Limited As our policy is one of continuous improvement, we reserve the right to modify designs without prior notice.
Visit our website for downloadable clinical & educational material and product information.
614469-3