Utah Medical Products
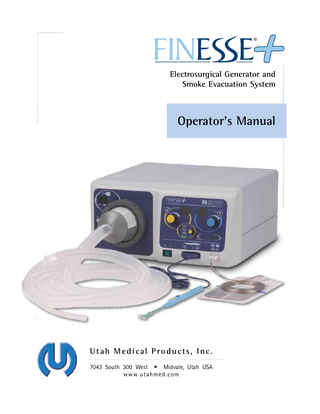
FINESSE+ Electrosurgical Generator and Smoke Evacuation System Operators Manual Rev 020713 July 2013
Operators Manual
58 Pages
Preview
Page 1
®
Electrosurgical Generator and Smoke Evacuation System
Operator's Manual
Utah Medical Products, Inc. 7043 South 300 West • Midvale, Utah USA w w w.ut ahme d.c om
Copyright © 2013 by Utah Medical Products, Inc. FINESSE®, UtahLoop® UtahBall®, Safe-T-Gauge®, DXTender®, LETZ®, and Epitome® are registered trademarks, and FINESSE+™, OptiMicro™, and ZapGuard™ are trademarks, of Utah Medical Products, Inc., Midvale, Utah.
Table of Contents Indications, Contraindications, Warnings, and Cautions Indications for Use 1
1
Contraindications for LETZ 1 Warnings 1 Cautions 4 Summary 5
Introduction 7 Description and Application 7 Electrosurgical Generator 7 Smoke Evacuation System 8 Electrosurgical Procedure Guidelines 8 The LETZ Procedure 10
Principles of Electrosurgery 15
Cutting 15 Coagulation 15 Complications 16 Smoke Evacuation and Filtration 16
Device Description 17
Front Panel Indicators and Connectors Rear Panel Controls and Connectors
17 21
Procedures 23 Initial Setup 23 Normal Operation 23 Maintenance 26
Troubleshooting 27 Technical Data 29 Physical Specifications 29 Supply Voltage and Current Considerations 29 Output Characteristics 30 Smoke Evacuator System 33 Environmental Specifications 34
Accessories 35 Glossary 37 Symbology 41
Electromagnetic Compatibility 43 Bibliography 47 Warranty and Service 49 Index 51 List of Figures and Tables Figure 1. Figure 2. Figure 3. Figure 4. Figure 5. Table 1. Figure 6. Figure 7. Figure 8. Figure 9. Table 2. Table 3. Table 4. Table 5.
FINESSE+ front panel, smoke evacuation module 17 FINESSE+ cut, coag, and error indication functions 19 FINESSE+ front panel connections 20 FINESSE+ rear panel connectors and controls 21 Dispersive electrode placement 24 Output Characteristics 30 Typical output power vs. load resistance for cut and blend modes 31 Typical output power vs. load resistance for coag mode 31 Maximum Output Voltage vs. displayed settings 31 Typical output power vs. display setting for cut and blend modes 32 and coag mode Symbols used in conjunction with the FINESSE+ System 41 Guidance and manufacturer's declaration - electromagnetic emissions 43 Guidance and manufacturer's declaration - electromagnetic immunity 43 Recommended separation distances between portable and mobile 45 RF communications equipment and the FINESSE+ System
Indications, Contraindications, Warnings, and Cautions CAUTION: Federal (USA) law restricts this device to use by or on the order of a physician or other licensed practitioner.
Indications for Use The FINESSE+ is intended to deliver high frequency electrical current for surgical procedures that can be performed with monopolar cutting and/or coagulation of tissue. One intended use of the Finesse+ system is Loop Excision of the Transformation Zone (LETZ®).
Contraindications for LETZ • • • • • • •
Positive ECC or a lesion in which the endocervical limit cannot be visualized colposcopically Clinically apparent invasive cervical carcinoma Pregnancy A bleeding disorder Severe cervicitis Less that six weeks postpartum DES-exposed patient.
Warnings WARNING: LETZ procedures should be performed by clinicians who are trained in diagnosis and management of cervical intraepithelial neoplasia (CIN). WARNING: Clinicians should be familiar with most recent clinical consensus guidelines regarding management of women with CIN when selecting patients for LETZ. WARNING: The following risks are associated with LETZ procedures: • Bleeding • Cervical stenosis • Infection • Incomplete excision of CIN • Pregnancy complications • Cautery artifact which may interfere with ability to evaluate margin of tissue specimen. Inspection. When the system is unpacked after transport between locations, as well as periodically with ordinary use, visually inspect the FINESSE+ system, accessories, accessory receptacles, power cord, and power cord receptacle for damage or missing parts. Do not use the system without correcting any observed or suspected damage.
1 FINESSE+ Operator’s Manual
No modification of this equipment is allowed. Modification of the FINESSE+ may expose operator and/or patient to hazardous electrical currents. Failure of HF surgical equipment can result in an unintended increase in output. Dispersive electrode pad. Always apply the dispersive pad as indicated in the dispersive pad instructions for use. Directions are provided with the dispersive pads. These directions should be rigorously followed to prepare, apply, maintain, and remove the dispersive electrode, and periodically make a visual check of the pad application to the patient. To ensure safe contact of the dispersive pad to the patient, use only pads listed as compatible with the FINESSE+'s CQM system. The use of contact monitoring pads that are not on the list in the Technical Specifications section of this manual may not properly signal an error condition and result in patient injury. If the patient moves after application of the dispersive electrode, the contact between the electrode and the patient should be rechecked before proceeding with the surgical procedure. Skin-to-skin contact (e.g. - between the arms and body of the patient) should be avoided, for example, by the insertion of dry gauze. This practice aids in preventing the establishment of alternate current paths. Grounding. At the frequencies and power levels used in electrosurgery, any grounded metal parts may conduct current away from the patient with sufficient concentration at the contact point to cause a burn. Although the isolated lead system of this generator is usually effective in limiting this leakage current and preventing such burns, there are circumstances where this precaution may be accidentally subverted and stray currents may flow. Therefore, the patient should not come into contact with metal parts which are grounded or which have an appreciable capacitance to ground (e.g. operating table, supports, etc.). The use of antistatic sheeting is recommended for this purpose. Jewelry. Jewelry can concentrate electrosurgical current if placed in the vicinity of the electrosurgical procedure or in the general path that the electrosurgical current would follow, for example, the path between the surgical site and the dispersive electrode. Also, loose fitting jewelry may come into contact with objects that could enable an alternate current path. Any of these conditions could cause patient shock or burn. Jewelry should be removed or isolated by dry gauze as much as possible. Leads. Unshielded active and return leads should be positioned so that they cannot come into contact with the patient or with other leads connected to the patient. They should also not be allowed to run closely parallel to other leads. Monitoring Leads. Electrodes and probes connected to monitoring, stimulating, or imaging devices (e.g. ECG electrodes) can provide paths for stray electrosurgical currents which may cause burns. This is possible even though these electrodes and probes are battery operated, insulated, or isolated at 50Hz/60Hz. The risk can be minimized by placing the electrodes or probes as far away from the surgical site and dispersive electrode as possible. Protective impedances in the monitoring leads can help reduce the risk of burns. Electrodes covering wide areas are best, and
2 FINESSE+ Operator’s Manual
needle-type monitoring electrodes should never be used during electrosurgery. In all cases, monitoring systems incorporating high frequency current limiting devices are recommended. Active Electrode. The surgeon handling the active electrode must, of course, avoid applying the active electrode to any point on his/her own body. The surgeon must also be aware that if the active electrode is touched to any conductive tool or appliance, that device becomes an extension of the active electrode and can cause burns to either the patient or the surgeon. When not being used, the active electrode should be stored isolated from the patient. Monopolar Electrosurgery. The FINESSE+ system is a monopolar type electrosurgical system. For surgical procedures where the HF current could flow through parts of the body having relatively small cross sectional area, the use of bipolar techniques may be desirable in order to avoid unwanted tissue damage. Accessories. Any reusable accessories should be periodically tested for function and safety in accordance with their manufacturers' instructions. Use only accessories whose connectors match those on the generator. Adaptors should not be used unless they are approved by Utah Medical Products as being compatible with the FINESSE+. The FINESSE+ system should only be used with the accessories that are offered by Utah Medical Products. However, it should be noted that certain accessories may appear to be physically compatible with the FINESSE+ system, but may not comply with quality and performance regulations, and as such may limit or impede the intended performance and safety features of the FINESSE+ system. To ensure that the FINESSE+ system complies with electromagnetic emissions and immunity regulations, users should use only the switchpens and dispersive pads listed in the Accessories section of this manual. Under no circumstances should switchpen cables exceed 10 ft (3m) in length, and dispersive pad cables should never exceed 10 ft (3m) in length. The use of accessories with longer cable lengths may result in increased emissions or decreased immunity of the FINESSE+ system. Only use active electrodes and pencils that have Rated Accessory Voltage greater than the Maximum Output Voltage for the selected output setting and mode (see Table 1 and Figure 8 in the Technical Specifications section). Power Deficiencies. The output setting selected should be appropriate for the intended purpose (see the section titled "Electrosurgical Procedure Guidelines"). Always use the lowest possible setting which achieves the desired excision quality and speed. An apparent power deficiency in cutting or coagulation may indicate faulty application of the dispersive electrode or failure of a patient lead. It may also result from attempting to push the electrode through the tissue faster than the natural speed of the electrode for the output level set inside the generator. If a slower cut does not produce the desired results, then the patient circuit, including the active and dispersive electrodes, should be checked before increasing the output settings. Sparks. The sparks generated in electrosurgical cutting or coagulation can easily ignite flammable substances at the surgical site. The use of flammable anesthetics or oxidizing gases such as nitrous oxide (N2O) and oxygen should be avoided if a surgical procedure is carried out in the region of the thorax or the head, unless these agents are drawn away. Non-flammable agents
3 FINESSE+ Operator’s Manual
should be used for cleaning and disinfection wherever possible. Flammable agents used for cleaning or disinfection or as solvents of adhesives should be allowed to evaporate before the application of the electrosurgical device. There is a risk of pooling of flammable solution under the patient or in body depressions such as the umbilicus and body cavities such as the vagina. Any fluid pooled in these areas should be removed before the electrosurgical equipment is used. Attention should be called to the danger of ignition of endogenous gases. Some materials, for example cotton wool and gauze, when saturated with oxygen may be ignited by sparks produced in normal use of the electrosurgical generator. Filters. After use, the external disposable filter can be a source of odor and possible viral contamination. Also, using this filter for too many procedures may compromise its particle or odor removal efficiency. For optimum performance, this filter should be discarded either daily or after 15 procedures if more than 15 procedures are performed in a single day. It should be removed with a gloved hand, placed in an appropriate plastic bag, and discarded with other plastic medical disposables. The internal filter, being protected by the disposable external filter pack, can withstand many more procedures than the external filter pack. It is recommended that this filter be replaced annually. See Annual Maintenance. The FINESSE+ system contains a special internal filter on the vacuum motor exhaust, which is designed to protect the internal electronics from particulate for the life of the system. Electromagnetic Interference. The FINESSE+ system has been tested to and certified to comply with recognized EMC (electromagnetic compatibility) standards to ensure proper operation when used near other electronic equipment, and that other similarly certified electronic equipment used near the FINESSE+ system should not be affected by it. However, users should take special precautions regarding EMC, and need to install the FINESSE+ system according to the EMC information provided in the Electromagnetic Compatibility section of this manual. Users should also note that portable and mobile RF communications equipment can affect medical electronic equipment. Electrosurgical generators may interfere with other electronic devices, particularly cardiac pacemakers. Precautions should be taken to ensure the patient's well-being in the event of such interference. These precautions should include: 1. Secure attachment of the dispersive electrode, 2. Placement of the dispersive electrode away from the heart, and as close as possible to the surgical site, 3. Other precautions as directed by the pacemaker provider. Note that the use of electrosurgery is contraindicated in patients implanted with certain cardiac pacemakers.
Cautions When installing the FINESSE+ system, do not choose a location where the FINESSE+ system will be adjacent to or stacked with other electromedical equipment. If operating the FINESSE+ system in close proximity to other equipment, observe the functioning of the FINESSE+ and other equipment to verify normal operation in the configurations that they will be used.
4 FINESSE+ Operator’s Manual
To avoid the risk of electric shock, the FINESSE+ system must be connected to a supply mains with protective earth (ground). To avoid damage to the power cord and receptacle, and if used, the footswitch cord and receptacle, keep the rear of the FINESSE+ system at least 3 inches (8cm) from all obstacles. Electric Shock Hazard. Unplug FINESSE+ system before cleaning, replacing internal filter, or removing fuse holders from the rear panel. If a single plug style pen is used, the user is not protected against inadvertent contact with the plug lead, which could result in electric shock and/or injury. CQM circuits used in electrosurgical generators are an excellent tool to minimize the risk of a patient injury during electrosurgery. CQM is effective at detecting changes in pad contact to the patient, and can signal the user to a potentially unsafe condition. However, these circuits should not be relied on as a method for detecting improper pad application or as a substitute for user attentiveness during the procedure.
Summary The FINESSE+ system has been designed to implement the best principles of electrical safety. The remaining burden for patient and operator safety lies with the user of the device. The most important safety factors that are under control of the operator are delineated above. It is important that these points, as well as others made throughout this manual, be read and understood before performing surgery with this instrument.
5 FINESSE+ Operator’s Manual
6 FINESSE+ Operator’s Manual
Introduction This manual is intended to: •
introduce you to the FINESSE+™ Electrosurgical Generator and Smoke Evacuation System,
•
acquaint you with the principles of electrosurgery,
•
make you aware of some important concerns inherent in electrosurgery, and provide instructions for operating this instrument in performing electrosurgical procedures.
Description and Application The FINESSE+ system combines a high-quality, class I type BF electrosurgical generator and a smoke evacuation system into a single compact unit. This integrated system was designed to perform low-power excision and coagulation procedures of short duration. It is not intended for high-power procedures such as prostatic resection or for sustained operating room procedures that require continual application of electrosurgical energy with only brief periods of rest.
Electrosurgical Generator The electrosurgical generator module in the FINESSE+ system is designed according to the same principles as the more powerful general surgery units that are commonly used in hospital operating rooms; however, its power output is limited to the range necessary for the shallower and less extensive cuts that are performed in office-based electrosurgical procedures. The output waveforms and load characteristics in the pure cut and blended cut modes are optimized for excisions in which the cut starts with only a small area of the cutting electrode in contact with tissue and proceeds to a maximum depth where the cutting line may be more than two centimeters long. The Controlled Output Circuitry of the FINESSE+ system is a negativefeedback output monitoring system that senses the changes in load resistance that occur throughout the excision and adjusts the power to match the needs of the cut. This prevents excessive tissue damage at the start and end of the cut and prevents slowing of the electrode when excising at the maximum depth. The FINESSE+ system provides a pure cut mode and three blend modes that perform concurrent cutting and superficial coagulation as required by standard practice for excision procedures. The coagulation mode provides sufficient voltage and power for spray coagulation, or fulguration, using ball electrodes. The generator incorporates an error detection and alerting system that will alert the user and shut down output power whenever the following occurs: 1. both cut and coag modes are simultaneously keyed ("cross-key" error), 2. a dispersive pad cable breaks or becomes disconnected
7 FINESSE+ Operator’s Manual
3. a split-type dispersive pad partially separates from the patient (CQM, or contact quality monitoring), or 4. the actual output power exceeds the set output by an unsafe margin.
Smoke Evacuation System The smoke evacuation system is integrated with the electrosurgical generator to enhance the convenience and safety of electrosurgical procedures, such as Loop Excision of the Transformation Zone (LETZ®). Its purposes are to remove the smoke that would otherwise obscure the visual field during the procedure, to filter particles from the smoke, and to adsorb the unpleasant odor. The smoke evacuation system consists of four major components: 1. a first-stage HEPA particulate filter 2. a second-stage activated charcoal filter 3. a third-stage ULPA particulate filter 4. a vacuum motor that creates the negative pressure and the resulting airflow necessary to pull the smoke from the surgical field and through the filters. The first two filter stages are supplied as a disposable unit (FINESSE Filter Pack, catalog no. ESU501) that may be easily changed and discarded. The third-stage ULPA filter and vacuum system are installed inside the FINESSE+ system housing. The ULPA filter (FINESSE+ Internal Filter, catalog no. SSE-500) is removable for annual replacement.
Electrosurgical Procedure Guidelines The surgical techniques using low-power generators are described in several medical journal papers and are being taught in current medical seminars. You are encouraged to learn the surgical methods from the established experts, then to read this manual carefully before using the FINESSE+ system and instruments to perform these procedures. A bibliography of papers on the subject is found later in this manual. Standard practice of these techniques may change as new findings are published. Because of the simplicity and low complication rate of electrosurgical excision procedures, some practitioners have elected to perform these procedures in their offices. The decision whether or not to follow this trend is the responsibility of the clinician. If the decision is made to perform the procedure in the office, the clinician should be aware that no surgical procedure is performed without risk and an appropriate degree of expertise must be developed to minimize these risks. It should also be noted that office procedures should be limited to those that do not carry significant risk of complications that may require emergency support. This criterion is met only when the excisions are not too deep and when they are performed using the same techniques that have been previously successful in the office environment. The developers and providers of the FINESSE+ system will not presume to prescribe surgical techniques in this manual. However, there are some guidelines and warnings that may be useful
8 FINESSE+ Operator’s Manual
in the process of the practitioner developing his/her own techniques. Some of these will be given in this manual. The output level settings appropriate for the various electrosurgical procedures are the first and most important parameters to be determined by the practitioner. The settings used by the developers of these techniques are given in their published papers. (Some of these papers are listed in the Bibliography section of this manual.) However, these published results were obtained using different electrosurgical generators. Every generator has its own cutting characteristics that may not be exactly duplicated by another generator using the same settings. Furthermore, the characteristics of the excision are dependent not only upon the output setting, but also upon the length and thickness of the cutting electrode, the moisture content and type of tissue, and the speed of the cut. Always use the lowest possible setting which achieves the desired excision quality and speed. WARNING: Cutting and coagulation of ex vivo tissue is NOT adequate training for performing LETZ or any other surgical procedure involving electrosurgical techniques. Users must obtain professionally recognized training in the techniques for diagnosis and management of CIN, including LETZ. The new user should develop confidence in the combination of the generator's characteristics and his/her own technique by practicing extensively on pieces of chicken breast or beef tongue. The objective of this practice is to determine the natural speed of the cutting electrode through the tissue at various output settings, and to observe how the depth of the thermal damage is influenced by the speed of the cut, the cut or blend mode selected, and the output setting used. After sufficient practice is obtained, the clinician should be able to develop the confidence and skill necessary to practice these procedures on patients using electrodes of different sizes and configurations for various procedures. Practitioners who prefer a slow cut, using a small electrode, or excising a small amount of tissue should use settings at the lower end of the output range. Those who prefer a faster cut, using a large electrode, or excising a large amount of tissue should use settings at the upper end of the output range. The cutting power required is dependent on many factors such as: 1. Nature of tissue to be excised. Fatty or cartilaginous tissues require higher power output than muscle or skin tissue. Sclerotic, fibrotic, or cicatrical tissues require higher power output than softer tissues. 2. Depth of excision. A deep excision (with the same electrode and speed of cut) requires a higher power output than a shallow incision. 3. Rate of speed at which the cutting electrode is moved. The faster the speed of the wire through the tissue during the cut requires higher power outputs than at slower speeds. 4. Type of electrode used. For a given depth of excision with an equivalent cutting speed, the longer wire requires higher power outputs than a shorter wire. Thicker wire requires higher power outputs than a thinner wire. 5. Tissue moisture content. Drier tissue requires higher power output than moist tissue.
9 FINESSE+ Operator’s Manual
The FINESSE+ generator diminishes the effects of some of the above variables by means of its feedback-controlled output. Because this circuit reduces the output power applied at the beginning and end of the cut to the minimum levels needed, it is generally operated at somewhat higher nominal output settings than most generators. The pure cut mode provides an excision with little hemostasis effect. Blend 1 provides an excision with minimal hemostasis effects. Blend 2 provides an excision with average hemostasis effect. Blend 3 provides an excision with maximum hemostasis effect. Coagulation of bleeding vessels after completion of an excision is usually accomplished using a ball electrode in the coagulation mode. In this mode, the ball electrode will throw sparks to the surface of the tissue with slight separation of the ball from the surface. This process, known as fulguration coagulation, should be done briefly to stop any bleeding that occurs. It should not be overdone. Other hemostatic techniques use the ball in contact with the tissue surface to coagulate by desiccation with little or no sparking. Desiccation techniques may cause unnecessarily deep thermal damage if not performed carefully. As with cutting, coagulation should be practiced on appropriate tissue simulators before performing the procedure on a patient. The coagulation power required is dependent on many factors such as: 1. Length of time the current is applied. Lower power outputs applied for longer periods produce a greater depth of coagulation than higher outputs applied for a shorter period of time. 2. Type of electrode used. A ball electrode will require a higher power setting than pointed electrodes, due to the larger area of tissue contact. 3. Character of surrounding media. Higher power outputs are required for coagulation under water or in a bloody field than for coagulation in relatively dry operative sites. For typical LETZ procedures, cutting mode output settings ranging from "40" to "70" have been found to be effective, with a setting of "65" typically used. Coagulation mode output settings ranging from "40" to "75" have been found to be effective in providing hemostasis for bleeding vessels, with a setting of "60" typically used.
Loop Excision of the Transformation Zone: The LETZ® Procedure NOTE: The following discussion of indications, contraindications, and procedure is merely intended to be a guideline for performing the LETZ procedure. The physician is encouraged to review this procedure and define his/her own protocol. Any recommendations listed are based on published articles but these articles, as well as other references listed in the Bibliography section of this manual, should be consulted and the physician’s protocol defined prior to performing the procedure. It should also be noted that the following information represents the thoughts in the LETZ procedure at the time that this document went to press. As with any medical procedure, the views and practices regarding the LETZ procedure may change. It is therefore recommended that the clinician maintain updated information on the procedure through the medical journals and/or other sources as the procedure continues to evolve. The LETZ procedure is a well-recognized method of treatment for Cervical Intraepithelial Neoplasia (CIN). Generally speaking, LETZ is acceptable for treatment of high-grade lesions (CIN 2
10 FINESSE+ Operator’s Manual
or greater), including suspected glandular abnormality, and for CIN 1 that is persistent at least 2 years, or is preceded by HSIL or AGC-NOS (atypical glandular cells - not otherwise specified) 2 1,2 cytology . The “2006 Consensus Guidelines” detail treatment recommendations for CIN, including management of CIN in “special populations” such as adolescents and young women, and should be consulted to provide the practitioner with a basis for their treatment decisions. 3 Treatment algorithms can also be obtained on-line. Contraindications for LETZ are detailed in Indications, Contraindications, Warnings, and Cautions. It is imperative to consider the risks and benefits of treatment versus non-treatment in 4 contraindicated patients.
LETZ Procedure and Technique It is recommended that the patient be provided with a brief description of the procedure and the equipment that will be used. ACOG, ASCCP, Utah Medical Products, and other professional organizations and equipment manufacturers have produced patient information brochures on the LETZ procedure that address many of the questions and concerns that your patients may have regarding the procedure.
Pre-Procedure Setup The supplies used for the LETZ procedure should be assembled prior to the procedure. These supplies may include, but are not limited to, the following list: • Acetic acid • Lugol’s iodine solution • Monsel’s solution • Saline solution • Vaginal speculum (non-conductive) with smoke evacuation port • Lateral vaginal wall retractor • Tissue forceps • Large and small cotton tipped swabs • Specimen container with preservation fluid • Local anesthetic (such as lidocaine 1% or 2% with or without epinephrine) with delivery system (including 25 to 27 gauge needle) • Loop and ball electrodes, various sizes in unopened sterile pouches • Dispersive pad • Electrosurgical pen • Smoke evacuation filter and tubing. Prepare generator system for use, with the exception of dispersive pad application and loop electrode selection and installation.
Performing the Procedure Place patient in lithotomy position. Place the vaginal speculum, with smoke evacuator tubing attached to smoke port.
11 FINESSE+ Operator’s Manual
Prepare the cervix for examination using acetic acid applied to a large cotton swab. Subsequently stain the cervical tissue with Lugol’s solution to enhance visualization of the lesion. If it is determined that the LETZ procedure is indicated, anesthetize the cervix. An intracervical block is typically used, injecting a total of 1.8 to 5.4 ml of lidocaine equally into four quadrants at a depth of about 2mm. The subsequent application of the dispersive pad will allow sufficient time 4 for the anesthetic agent to take effect (typically 3 minutes). Apply dispersive pad to the patient. Complete application of the entire surface of the dispersive pad should be visually verified. Always review the dispersive pad instructions for use before applying the pad. For the LETZ procedure, consider the following recommendations for placement: • Place the dispersive pad on the thigh of the leg closest to the FINESSE+ system. • Apply the pad to the upper thigh, anterior. • Orient the pad so that the cord faces outward from the patient, toward the FINESSE+ system. • Take care to avoid pad application in areas containing folds, hair, scar tissue, or dry or oily skin. • Apply the pad by smoothing the pad from one edge to the opposite edge, in order to ensure that the full surface of the pad is adhered to the patient’s skin. Activate the FINESSE+ system’s main power switch. 4,5,6
The loop electrode should be selected, keeping the following needs and guidelines in mind: • If possible, the loop should be wide enough to completely remove the lesion in one pass, plus allow for an adequate margin of healthy tissue so that the squamocolumnar junction can be identified by the pathologist. • An irregular shaped lesion, or a lesion that extends into the endocervix, may indicate that more than one pass of the loop electrode and/or the use of more than one size of loop electrode will be needed. • The endocervix is commonly not included in the loop excision, and the results of endocervical curettage (ECC) do not appear to be predictive of either residual or invasive disease after a loop excision procedure. If the ECC is positive for dysplasia, a cone biopsy should be considered. • CIN does not typically penetrate more than 6-8mm below the surface of the cervix, therefore the excision depth should be closely monitored to avoid excessive removal of healthy tissue, yet ensure complete removal of the lesion and involved glands. Excessive removal of tissue could result in cervical stenosis, yield fertility and pregnancy effects, or have other complications. Insert the loop electrode into the electrosurgical pen. Perform a “test pass” to ensure that the excision path is unobstructed. Perform the loop excision. • It is recommended that the cut mode output be activated just before the loop makes initial contact with the tissue.
12 FINESSE+ Operator’s Manual
• •
•
Unless necessary, do not deactivate output power during the excision. If the loop “stalls” or output power is otherwise interrupted, the loop electrode should be removed from the tissue and the cut restarted from the opposite side of the planned excision. The excision should be performed from left to right or from right to left. However, if it is indicated, posterior to anterior motion may be used to remove the most suspicious areas of the lesion in the first pass. It is not recommended that the excision be performed from anterior to posterior, as the pooling of blood from the excision will tend to excessively dissipate the output power. This may cause the loop to “drag” and may result in excessively deep thermal damage to the tissue. Attempt to maintain the speed of the loop through the excision. Moving the loop too slow or too fast may result in excessive thermal damage to the tissue. The speed of the loop through the tissue during the excision should not be so fast as to cause the loop wire to bend back; the loop should excise the tissue with little mechanical resistance, yet still be fast enough to avoid excessive delivery of power to any given localized area of tissue.
Remove the tissue specimen using tissue forceps, mark for orientation, and place into container with preservative fluid. Label the specimen vial accordingly. Inspect the excision bed and the endocervical canal for residual CIN, as well as ensuring that no endocervical glands remain in the excision bed. Remove the loop electrode and insert the desired ball electrode into the electrosurgical pen. Perform fulguration coagulation to control bleeding. Fulguration coagulation is the preferred method, as desiccation coagulation tends to cause deeper thermal tissue modification. Monsel’s solution may be used in the excision bed as a hemostatic agent following fulguration. The Monsel’s solution should be a gel or paste, and is applied using a cotton swab only to the excision bed. Monsel’s should not be applied to adjacent areas of tissue. Dispose of the used electrodes, dispersive pad, and electrosurgical pen.
Post-Procedure Guidelines Instruct the patient on post-procedure care and attention. These recommendations may include: • Avoid lifting heavy objects, using tampons, douching and vaginal intercourse for 3 to 4 weeks. • Bleeding and a dark discharge are normal, but heavy bleeding, with blood loss typical of menstruation, should be reported to the physician. • Bleeding that occurs more than two weeks post-procedure should be reported to the physician. • A malodorous discharge which may or may not be associated with pelvic pain should be reported to the physician. • Instruct the patient to return to the office in three to six months for a follow-up Pap smear and/or colposcopy.
13 FINESSE+ Operator’s Manual
References 1. Wright TC, Massad LS, Dunton CJ, et al, 2006 consensus guidelines for the management of women with abnormal cervical cancer screening tests, Am J Obstet Gynecol, 2007; 197(4):34655. 2. Wright TC, Massad LS, Dunton CJ, et al, 2006 consensus guidelines for the management of women with cervical intraepithelial neoplasia or adenocarcinoma in situ, Am J Obstet Gynecol, 2007; 197(4):340-45. 3. “2006 Consensus Guidelines for the Management of Women with Cervical Intraepithelial Neoplasia or Adenocarcinoma in situ.” American Society of Colposcopy and Cervical Pathology (ASCCP). October 2007. Available at http://www.asccp.org/Portals/9/docs/pdfs/Consensus%20 Guidelines/algorithms_hist_07.pdf. Retrieved June 27, 2012. 4. Electrosurgery for HPV-related diseases of the lower genital tract, Wright TC, Richart RM, Ferenczy A, Arthur Vision, Inc., New York, 1992. 5. Large loop excision of the transformation zone, Prendiville W, Chapman & Hall, 1993. 6. Baggish MS, Ferenczy A, Gerbie M, Richart RM, Potential complications of loop excision, Contemp OB/GYN 1994: 39(8):93-107.
14 FINESSE+ Operator’s Manual
Principles of Electrosurgery The FINESSE+ system is a monopolar generator which produces the optimal waveforms for electrosurgical cutting and coagulation. In monopolar electrosurgery, a radio frequency current is passed through the body of the patient between an active electrode, where the current is very concentrated, and a dispersive electrode, where the current is quite diffuse. The active electrode is used as a cutting or coagulating tool at the site where surgery is to be performed. The dispersive electrode is applied at a site away from the surgical field for the purpose of returning current to the generator. Electrosurgery results from the concentration of electrical energy in tissue to the point that the tissue is locally destroyed or modified. In electrosurgical cutting, the cells conducting the concentrated current are heated to the point where the water contained inside the cells boils and the cells explode to release steam. In electrosurgical coagulation, cells near the surface are heated so that those not exploded are dehydrated and shrunk to the point where open vessels are closed.
Cutting To obtain cutting with minimal heating, a tool with a small cross section, such as the thin-wire loop, is driven with an electrical source having a continuous, unmodulated wave form. This kind of power source is referred to as a pure cut source. Modulating or periodically interrupting the voltage from the cutting source creates a current that will cause shallow surface coagulation as well as cutting. This kind of source is called a blended source. The FINESSE+ system has a pure cut mode and three blended cut modes. The waveforms produced to provide these modes are described quantitatively in the Technical Data section of this manual.
Coagulation To obtain coagulation without cutting, an active electrode with a larger cross section, such as a ball electrode, is usually used. A power source with a high voltage interrupted waveform is applied to the active electrode. Fulguration is accomplished using either a blunt or fine electrode with the coag mode waveform. The active electrode is held slightly above the surface to be coagulated so that the sparks jump across the gap. At the points on the surface where the sparks enter, very high current densities are achieved and tissue is seared. However, the area of the surface contacted by the spark and the current carried by each spark are small and the heat damage is quite shallow. This method usually produces a good cosmetic result after healing is complete.
15 FINESSE+ Operator’s Manual
Complications When an appreciable electrical current is caused to flow through the patient's body, as in all monopolar electrosurgery, the common undesirable physiological effects of electric current must be considered. In the above discussions of electrosurgical theory, such words as cutting, cell explosion, burning, sparking, and searing have been used. Any of these phenomena occurring too strongly or at the wrong places are undesirable. In addition to these, there is also electric shock, which has not yet been considered. Electric shock, or faradic effect, results from the depolarization of nerve or muscle cells by a nonphysiologic electric voltage. In electrosurgery, this effect is avoided by using voltage waveforms of such high frequencies that the ions, which must migrate across a cell membrane to depolarize a cell, are only caused to vibrate over very small magnitudes. Heat is dissipated, but shock does not occur. To avoid electric shock, frequencies above 300,000 cycles per second (300 kHz) must be used. The FINESSE+ system operates at 450 kHz, which is well above this limit. The other undesirable effects of electrical current, such as burns, are avoided by proper design of the generator, careful application of the dispersive electrode, maintenance of the patient contact with the dispersive electrode, and avoidance of all metallic contacts to the patient that may allow alternate paths for the electrosurgical current. The FINESSE+ system has been designed with isolated patient leads which minimizes the potential for currents to seek alternative routes. It also provides error indicators to signal when the dispersive electrode's connections are broken and patient contact possibly compromised. There remains the possibility that the isolation may be destroyed by inadvertent direct or capacitive grounding in the patient connections outside the generator. The warnings and precautions given in the Operational Safety Notes and Warnings section of this manual must be strictly heeded.
Smoke Evacuation and Filtration The smoke produced during electrosurgery has an odor that is unpleasant, strong, and persistent. It consists of organic gases, water vapor, visible and sub-visible solid particles and virus particles. It is generally considered good practice to remove the smoke from the surgical field and filter it. A system for this purpose is provided as part of the FINESSE+ system. Filtering of the smoke is accomplished using a HEPA (High Efficiency Particulate Air) pre-filter, a layer of activated charcoal, and a third-stage ULPA (Ultra Low Penetration Air) particulate filter. The effectiveness of the two stages of particle filtering has been measured on several filters using spherical latex particles. The combined particle filtration efficiency of both filters was found to be equal to or better than 99.999% efficient on 0.1 micron particles. The vacuum motor used in the FINESSE+ system produces sufficient pressure reduction to pull approximately 70 liters per minute (2.5 cfm) at the normal setting through a 30cm long smoke tube with a 6mm inside diameter. This rate is effective in removing smoke from an enclosed surgical field as required by the LETZ procedure. It should be noted that a smaller diameter tube will significantly reduce the flow rate. Also, it is easier for smoke to escape from an open surgical field. It may be necessary to switch to the "high" flow setting to achieve effective smoke removal under these circumstances.
16 FINESSE+ Operator’s Manual